What is Brachial Plexus Birth Palsy (BPBP)?
Brachial Plexus Birth Palsy (BPBP) occurs when the network of nerves controlling movement and sensation in the shoulder, arm, and hand, known as the brachial plexus, is injured during birth (Figure 1).
These nerves can be stretched, compressed, or even torn due to traction on the baby’s neck and shoulder area, especially in challenging deliveries.
This injury can lead to weakness, limited movement, and varying levels of sensation in the affected arm.
In most cases, partial or full recovery occurs with early treatment, but some children experience long-lasting effects, including shoulder dysplasia.
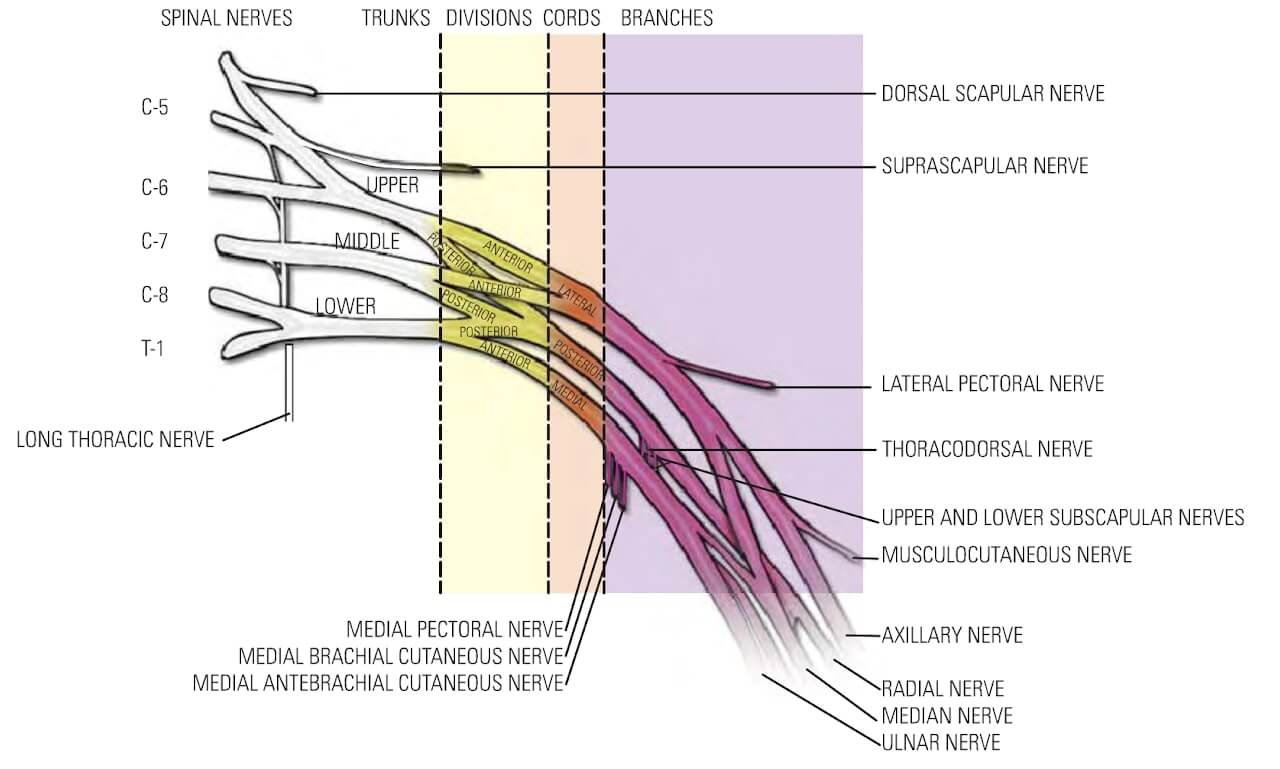
Figure 1: Anatomy of the Brachial Plexus
How and Why is the Shoulder Joint Affected in BPBP?
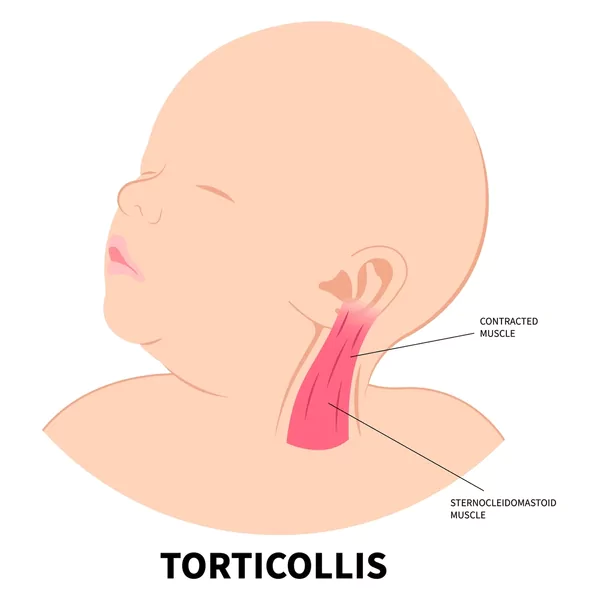
The brachial plexus nerves supply signals to the muscles of the shoulder, allowing for stability and a full range of motion. When these nerves are injured, certain shoulder muscles do not receive sufficient nerve signals, causing an imbalance in muscle strength.
This imbalance can lead to abnormal shoulder joint development and dysplasia, as muscles critical for outward rotation and alignment weaken.
Over time, this leads to shoulder joint malformation or dysplasia, where the socket of the shoulder is underdeveloped, often creating a deformity that can further impact function.
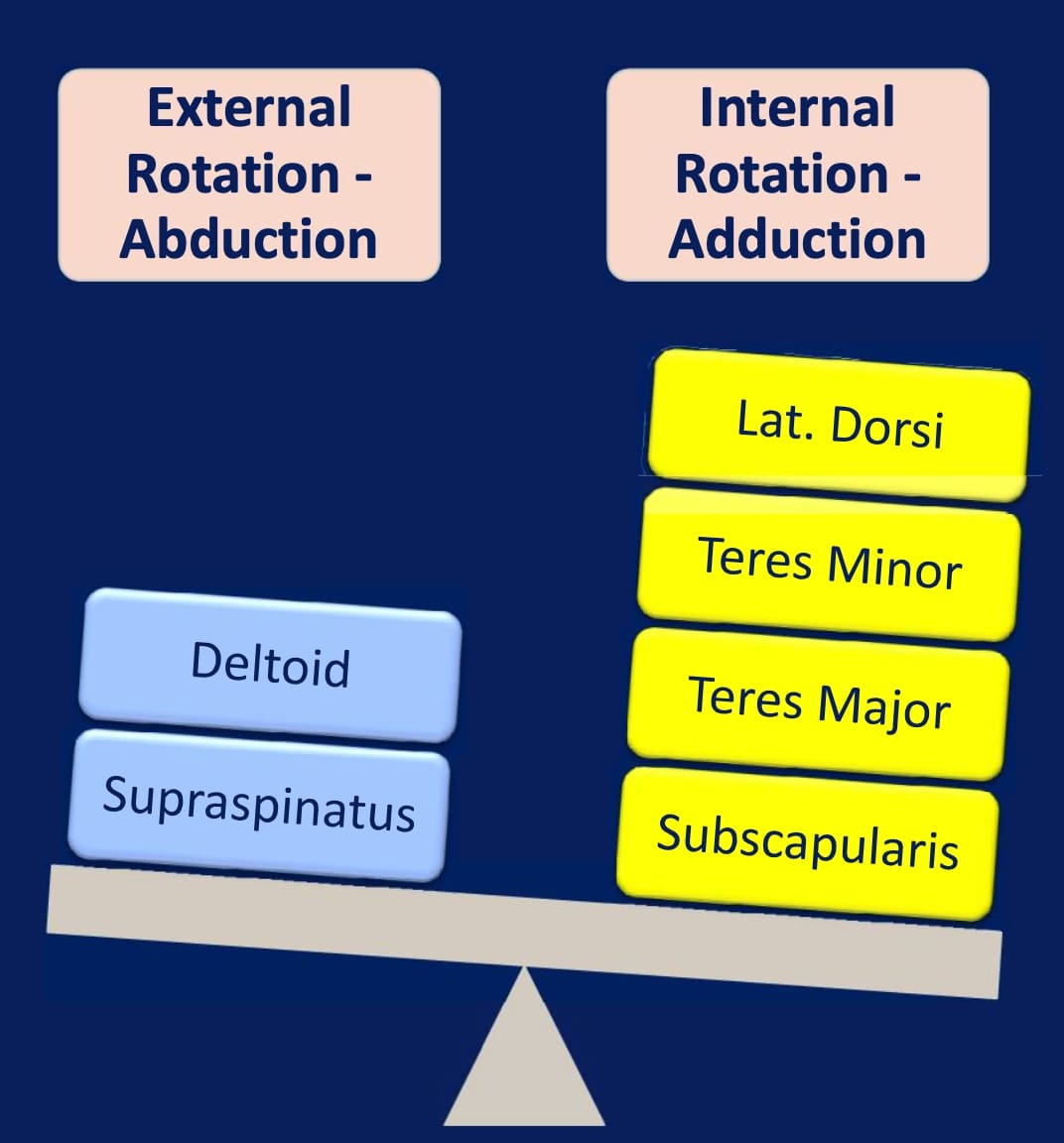
Figure 2: In partially recovered Brachial Plexus Birth Palsy, the fully recovered internal rotator muscles overpower the weakened external rotators
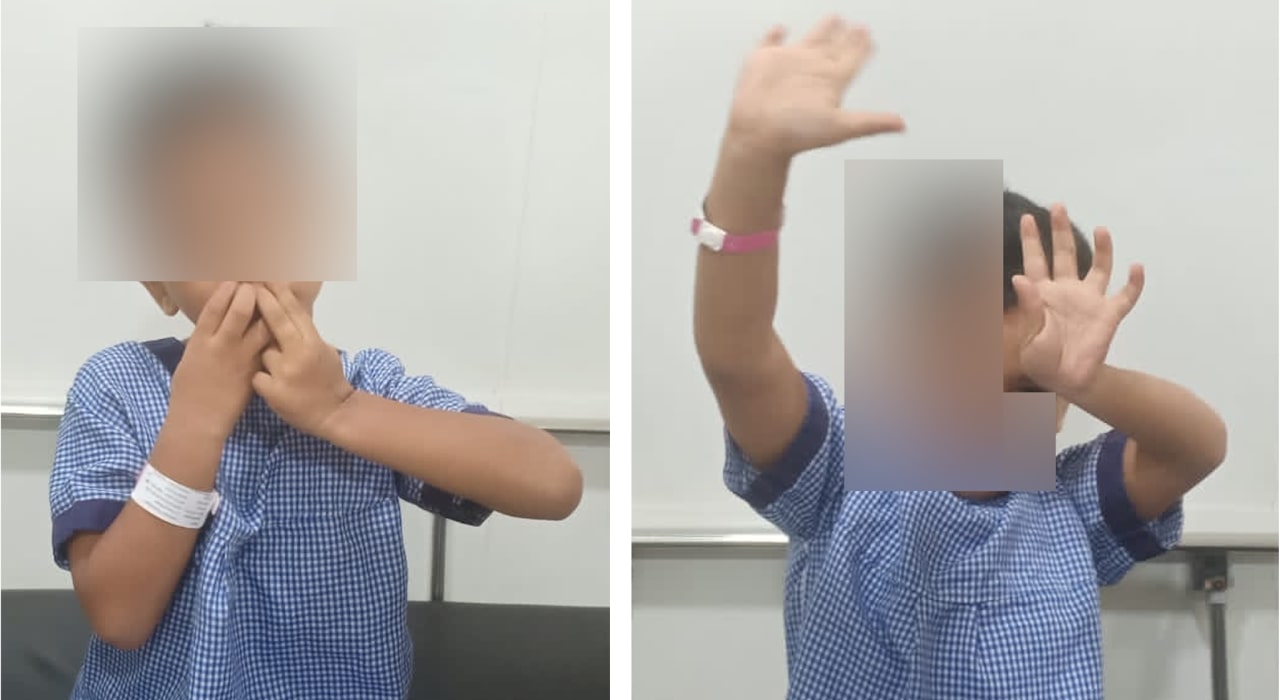
What are the clinical signs of shoulder joint problems in BPBP?
Children with shoulder involvement in BPBP may struggle with specific movements, particularly outward rotation or raising the arm. The child has difficulty in performing hand to mouth activities and raises the shoulder in a typical “trumpet holding position”. The child may also face difficulty lifting the arm above shoulder level.
What investigation helps in diagnosing shoulder joint problem in BPBP?
MRI is the most useful diagnostic tool in BPBP cases with suspected shoulder dysplasia. MRI is especially helpful in planning surgery, as it reveals how much of the joint and muscles are affected, assisting the surgeon in determining which structures need intervention.
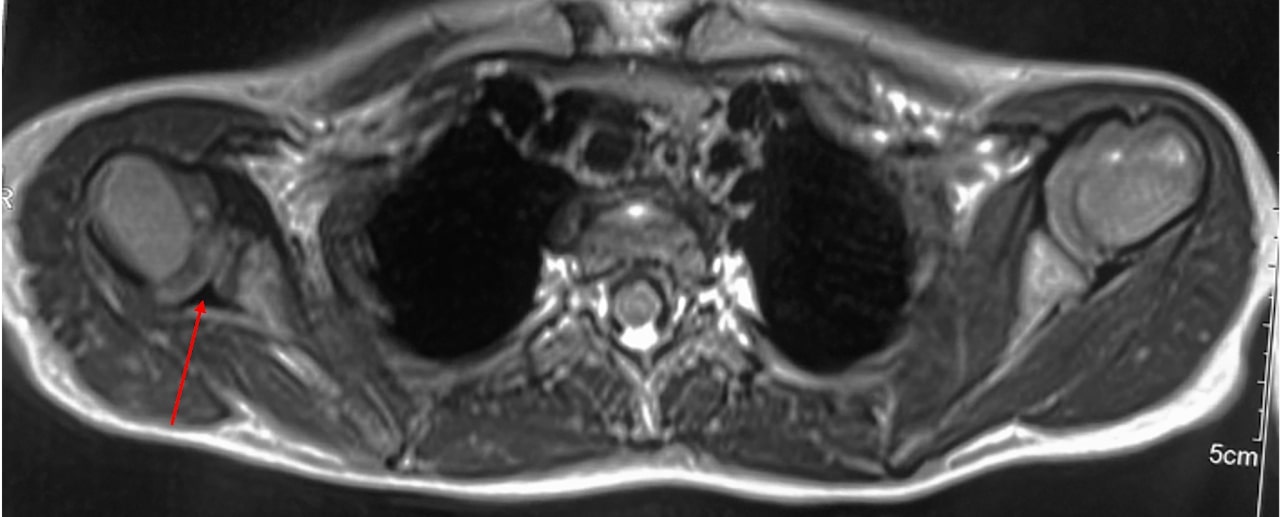
Figure 4: MRI is the imaging modality of choice to diagnose shoulder joint pathology in BPBP
What is the treatment if shoulder joint affection in BPBP?
When shoulder dysplasia and internal rotation contracture (where the shoulder remains inwardly rotated) are severe, surgical intervention may be needed. An anterior shoulder release with muscle transfer surgery is a common approach to improving alignment and movement.
The surgery focuses on releasing the tight structures causing the shoulder to rotate inward and transferring specific muscles to enhance outward rotation, aiming to restore a balance in shoulder function.
This surgery aims to restore the muscle balance around the shoulder, , giving the child a chance to develop a normal shoulder joint over time.
What is the post-operative protocol after shoulder muscle transfer surgery in BPBP?
After surgery, the shoulder is immobilized in a special cast that holds it in the desired position to allow the transferred muscles to settle and heal. The cast maintains the new shoulder alignment, giving the muscles time to adjust and reducing the likelihood of further contracture. Immobilization generally lasts about 4 weeks.
Once the cast is removed, rehabilitation is essential to build strength, improve range of motion, and encourage the use of the affected shoulder. Physical therapy includes exercises that focus on gentle stretching and strengthening. Splints may also be used to hold the shoulder in a favorable position while the child is not actively exercising.
A structured rehabilitation program encourages gradual use of the arm and shoulder in daily activities, ensuring the child becomes comfortable with the new movement patterns.

Figure 5: After surgery, plaster cast is applied for a period of one month. This is followed by a period of sleeptime splint wear for few months.
What are the expected outcomes and functional improvements after shoulder muscle transfer surgery in BPBP?
Most children undergoing shoulder anterior release and muscle transfer surgery experience notable improvements in shoulder alignment, range of motion, and function. They often find it easier to raise their arm, rotate it outward, and perform tasks like dressing or reaching for objects with the affected arm.
While the degree of improvement varies, this surgical approach significantly enhances the child’s quality of life by restoring function, making them more independent in daily tasks.
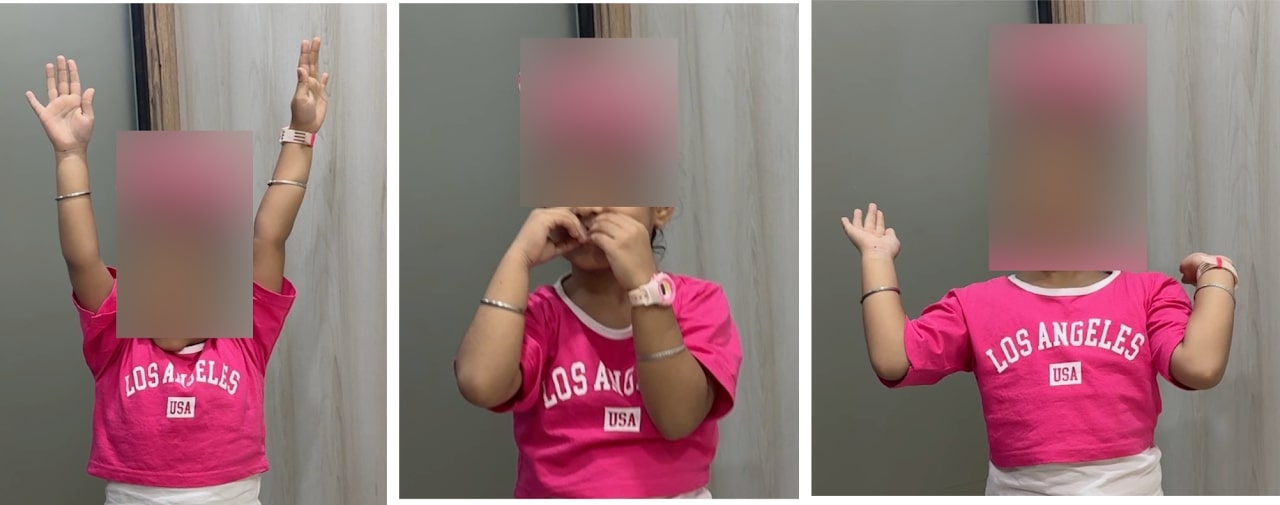
Figure 6: Improvement of shoulder overhead, hand to mouth and external rotation activities after shoulder surgery for BPBP
Conclusion:
With a balance of clinical understanding and supportive therapy, children with BPBP can achieve significant functional gains, offering families hope for their child’s independence and quality of life.
_ By Dr Sandeep Vaidya, Paedictric Orthopaedic Surgeon, Pinnacle Orthocentre Hospital. For more information, mail drsvvaidya@gmail.com/ call 7028859555.



0 Comments