Introduction
‘Cerebral Palsy’ (CP) is a disorder that affects a child’s ability to control his/her muscles. It is caused by damage to parts of the immature brain that control movement and coordination. The brain damage in cerebral palsy is non-progressive, unlike brain tumors and neurodegenerative disorders which are progressive. However, the deformities that occur in the limbs secondary to the brain damage can be progressive as the child grows older.
Types:
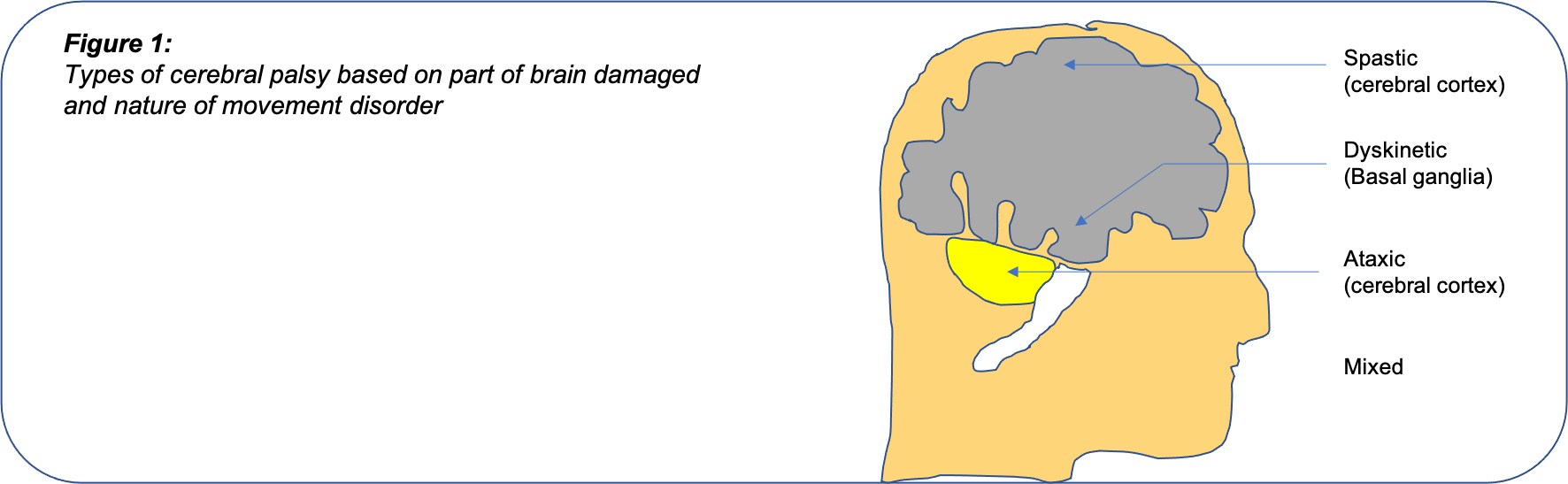
Depending on the part of the brain affected, cerebral palsy can be:
- Spastic cerebral palsy: This is the commonest form and occurs due to damage to the cerebral hemispeheres. In this type, the affected muscles are spastic. i.e. they are very tight and do not relax easily.
- Dyskinetic cerebral palsy: This form of cerebral palsy occurs due to damage to the basal ganglia. In this form, the child’s arms or legs repetitively move in abnormal twisting movements. This may occur whenever the child attempts to use the arm/ leg or may even occur continuously when the child is at rest.
- Ataxic: This form of cerebral palsy occurs due to damage to the cerebellum. This is characterized by unsteady gait pattern and loss of balance while walking
- Hypotonic: In this type, the limbs are limp and floppy. This is usually seen in young infants but gradually evolves into spastic type as the child grows older.
- Mixed: This is seen when the brain damage is more extensive. Components of more than one type of cerebral palsy are seen in mixed cerebral palsy.
Depending on the parts of the body most affected, cerebral palsy can be:
- Hemiplegic: When one half of the body i.e., the upper and lower limbs on either the Right or Left side are affected.
- Diplegic: Both lower limbs are more severely affected than the upper limbs.
- Quadriplegia: This is the severest form, in which both upper and lower limbs are equally affected. There is associated weakness and loss of control of the trunk. Children with this form of cerebral palsy are often non-ambulatory and bed-ridden.
Depending on the severity, Cerebral Palsy is classified according to the Gross Motor Function Classification System (GMFCS) as:
- Level 1: Can walk and climb stairs without support, however, have decreased speed and balance while running and jumping.
- Level 2: Can walk without support, however, need to hold railing while climbing stairs. Cannot run or jump.
- Level 3: Need support of walker/ crutches for support. Cannot climb stairs. Need a wheelchair for long distances or uneven terrain.
- Level 4: Are capable of standing for transfers, however, need a wheelchair for ambulation.
- Level 5: Poor trunk and head control. Cannot sit independently.
Causes:
Cerebral Palsy occurs due to some damage to a small child’s growing brain. This damage may be:
- Pre-natal: Brain damage occurs while the child is in the womb. If the mother is ill or is exposed to some toxins during pregnancy, and also when the child’s brain fails to develop normally.
- Peri-natal: Damage occurs around the time of birth. Babies who are born prematurely or who have a very low birth weight, or those who do not breathe immediately after birth and need ventilator support, or those who develop jaundice or severe infections or bleeds in the brain, are prone to develop cerebral palsy.
- Post-natal: Damage may occurs soon after birth. Babies who have trouble breathing and need to be kept on a ventilator, those who suffer from jaundice, or have bleeds in their brain, and al who suffer head injuries or ischemic brain damage due to drowning in the first three years of life may develop cerebral palsy.
All these are the known risk factors for CP, however the exact cause may not be known in many cases. Many children who have the above risk factors around birth do not go on to develop CP, whereas some children who have completely normal births may go on to have CP.
Symptoms:
The initial symptom of CP is usually a child who is slow to meet his/her developmental targets. The normal timing of achievement of motor milestones are as under:
- Neck-holding: 3 to 4 months
- Rolling over: 4 to 6 months
- Sitting up: 6 to 8 months
- Crawling: 8 to 10 months
- Standing with support: 10 to 12 months
- Walking with support: 10 to 14 months
- Walking without support: 12 to 18 months
Gross delay in the achievement of these motor milestones should be evaluated to rule out Cerebral Palsy or other neurological conditions.
CP also affects other body systems besides the movement problems:
- Learning disabilities
- Speech problems
- Epilepsy (seizures or fits)
- Visual problems
- Hearing difficulties
- Problems with swallowing, constipation
- The curvature of the spine and poor posture
- Joint problems like hip dislocations
Diagnosis:
There is no single investigation that can diagnose Cerebral Palsy. The diagnosis is reached after careful evaluation of history, clinical examination, walking pattern, and special investigations like MRI of the brain. MRI is normal in approximately 20% of children with cerebral palsy. Additionally, your doctor may advise tests to rule out other neurological conditions which may mimic Cerebral Palsy
Treatment:
Team:
Management of a child with Cerebral Palsy is a team effort. Specialists who should be involved in the treatment of a child with Cerebral Palsy include:
- Paediatrician
- Paediatric neurologist
- Physiotherapists: To help improve movement and strength
Additionally, depending on the specific problems that your child has, you may also need to consult a number of other specialists:
- Pediatric Orthopaedic surgeons: to treat the problems with muscles, bones, and joints
- Eye specialists: For visual problems
- Ear, nose, throat (ENT) specialists: For problems in hearing
- Occupational therapists: To help your child learn daily living skills such as eating, dressing
- Speech therapists: To help with communication problems
- Nutritionists: To help give your child the type of diet he/she needs
- Orthotists: To provide braces and aids to help your child walk and do other activities
- Special teachers
Spasticity Management:
Spasticity management in a child with Cerebral Palsy consists of a combination of medications, physical therapy, bracing, and surgery.
Medications: Your pediatrician/neurologist will prescribe medications to help reduce the excessive tightness in your child’s muscles. Medicines may also help, to an extent, to reduce the involuntary twisting movements in children with dystonic CP. Many children with CP also suffer from epilepsy and require anti-epileptic therapy.
Physical therapy: Physiotherapy and occupational therapy are required for children with CP throughout their growing years. It is needed to help stretch out tight muscles and to strengthen muscles that are weak. Children with CP need to be specially taught how to do daily activities like walking, dressing, etc. These activities do not come naturally to them as they do for other children, because the weakness and tightness in their muscles make it very difficult for them to perform any task.
Bracing: The use of braces and splints is necessary to place the joints in a functional position. They improve balance and reduce the effort of walking. Splinting, especially at night, keeps the muscles stretched out, and is thus helpful in preventing or at least delaying the need for surgery.
Injection Botulinum Toxin:
‘Botox’ or ‘Botuminum toxin’ is a chemical that relaxes tight muscles when injected into them. It is often used in CP, for children who’s muscles are very tight. The effect of botox lasts for 6 months, hence, the injection may need to be repeated. However, if you regularly do physiotherapy and use the necessary braces, the beneficial effects of botox can be prolonged by several months. Botox is only beneficial when the involved muscles are tight, but not rigidly fixed in that position.
Surgery:
The judicious use of surgery has an important role in the treatment of CP. However, do remember that CP covers a very broad spectrum, and each child with CP is unique. Accordingly, the need for surgery will depend on many factors. In most children, surgery is not required until they are older. Regular exercise and use of braces can help in delaying the need for surgery, however, most children with severe CP need surgery eventually.
When tight muscles become rigidly fixed, then the child’s joints become fixed in abnormal positions. This is called a ‘contracture’. Once developed, contractures cannot be relieved by physiotherapy, braces or even injection of Botox. In such cases, surgery is needed to release the tight muscles, so that the joints can return to a functional position.
Sometimes, the contractures around a joint are so severe, that they actually cause the joint to dislocate. This is most commonly seen at the hip in CP. When the hip is dislocated, the child’s leg is tightly pulled towards the opposite leg, making it difficult to clean your child, and apply his/her diaper. It also makes it difficult for the child to sit, and can be painful. In such cases, surgery is required to restore the joint to normal.
Children with CP often have persistent rotational abnormalities in their bones that can make walking difficult. Such children benefit from surgery to cut the bone and turn it into a more functional position.
Prognosis:
The injury in the brain which results in CP remains the same and does not change over time. However, as the child grows, the problems with movement and other impairments do change. As your child’s body becomes bigger, the muscles which are already tight and weak are not able to keep up with the bones that are growing rapidly. As a result, the weakness in certain muscles worsens. Also, the tight muscles which could earlier be stretched out with exercise and braces now become fixed. Rapid growth also causes worsening of curvatures of the spine (scoliosis).



0 Comments