What is Developmental Dysplasia of Hip?
The hip joint is a ball and socket joint in which the femoral head (ball) articulates with the acetabulum (socket) (Figure 1).
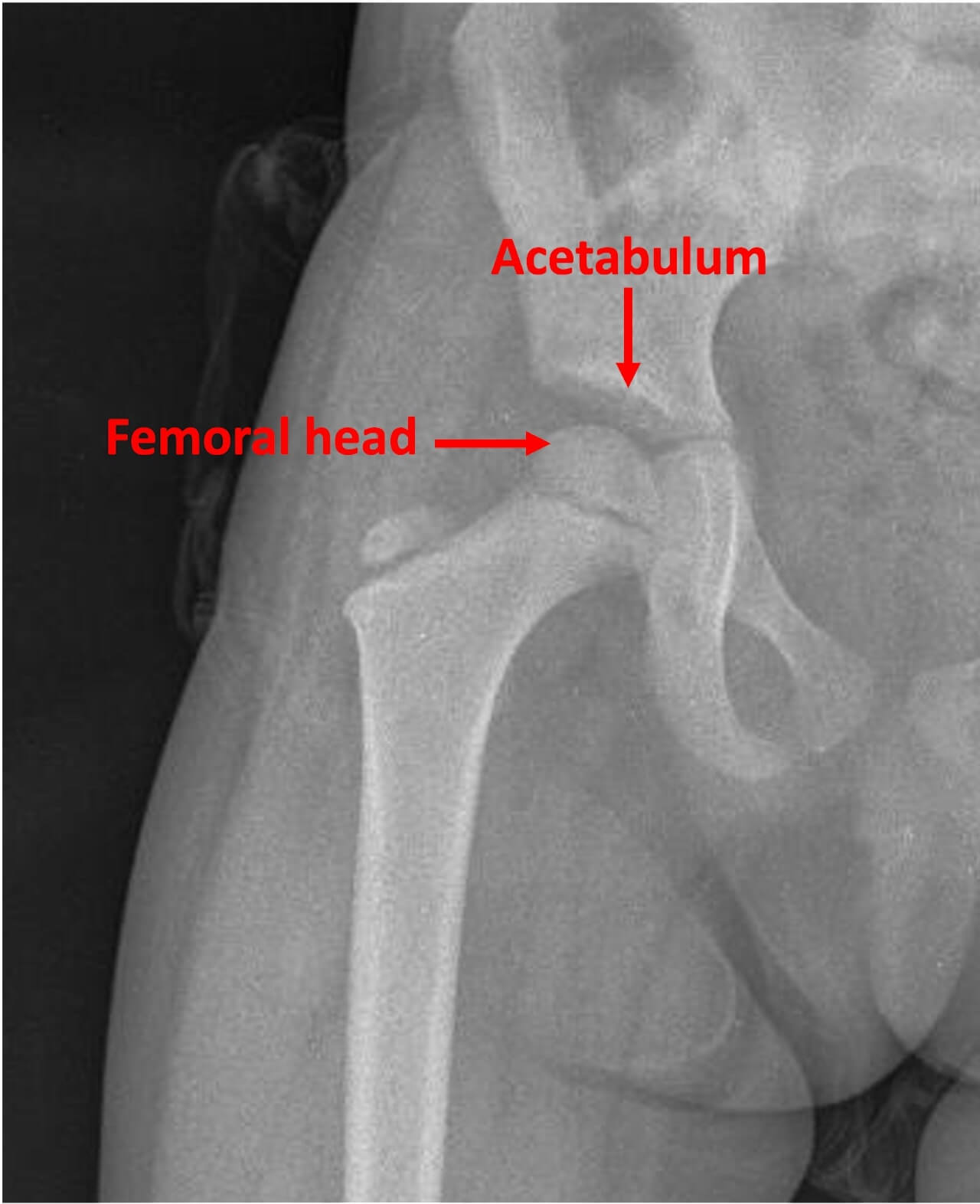
Figure 1: The hip joint is a ball-and-socket joint.
Developmental Dysplasia of Hip (DDH), in simple terms, is a pathology in which the socket (acetabulum) is shallow. DDH can present with a spectrum of severity.
In the mildest form (dysplasia), the acetabulum is shallow but the femoral head is located within the acetabulum. In subluxation, the femoral head is partially displaced out of the acetabulum.
In the severest form (dislocation), the femoral head is completely out of the acetabulum (Figure 2).

Figure 2: Spectrum of severity in DDH
Why is the need felt for the implementation of screening program for DDH?
Treatment of DDH is age-based. If diagnosed before the age of 6 months, treatment by Pavlik harness is usually successful. In 6 months to 1 year age group, Closed reduction and hip spica application under anaesthesia is usually needed.
In children more than 1 year age, surgery is needed. It is thus clear that as the age at diagnosis increases, the complexity of treatment increases.
Furthermore long term studies have shown that outcomes of surgical intervention for DDH are inferior as compared to treatment with Pavlik harness (Figure 3).
Due to this importance of early diagnosis, there is a perceived necessity for the implementation of screening program for DDH.

Figure 3: Treatment of DDH is age based and becomes progressively more complex as the child’s age increases
DDH screening in Western countries:
Due to the importance of early diagnosis, most Western countries have implemented nation-wide screening programs for DDH. Data from these countries shows that screening helps in early diagnosis, decreases the incidence of late detected DDH, which in turn helps to decrease need for surgical intervention.
Most of the screening programs implemented in Western countries depend on the Ultrasonography (USG) diagnosis of DDH.
Problem in India: The need for India specific guidelines
Screening programs from Western countries can’t be simply aped in India due to the limited availability of resources (USG) and expertise (trained sonologists) in the remote parts of the country.
In the absence of a formal screening program, India continues to see a significantly higher disease load of late detected DDH. Consequently the incidence of surgery for DDH is also significantly higher in India.
It is against this backdrop that the need was felt formulate Indian surveillance guidelines which would take into account indigenous ground realities and which can be uniformly applied all across the country.
Formulation of Indian DDH surveillance guidelines:
With this objective in mind, members of 7 professional bodies: The Pediatric Orthopaedic Society of India (POSI), Indian Academy of Pediatrics (IAP), National Neonatology Forum of India (NNFI), Indian Radiological and Imaging Association (IRIA), Indian Federation of Ultrasound in Medicine and Biology (IFUMB), Federation of Obstetric and Gynaecological Societies of India (FOGSI), and Indian Orthopaedic Association (IOA) formed a multi-disciplinary expert group.
They were ably supported in this endeavour by the International Hip Dysplasia Institute (IHDI), a not-for-profit organisation based out of USA and Canada, working towards raising awareness of DDH (Figure 4).

THE INDIAN HIP SURVEILLANCE GUIDELINES 2022:
After rounds of discusseions, the group formulated consensus guidelines for surveillance for Developmental Dysplasia of Hip (DDH) in infants in India. The guidelines were published in the August 2022 issue of Indian Paediatrics (click here to access full-text of the article).
In this blog article, let’s summarise these guidelines:
QUESTION 1: WHO SHOULD UNDERGO SURVEILLANCE FOR DDH?
All neonates, without exception, should undergo surveillance for DDH.
QUESTION 2: WHEN SHOULD DDH SURVEILLANCE BE PERFORMED?
Note that the Indian guidelines emphasise the term “hip surveillance” in lieu of “screening”. This signifies that hip examination needs to be performed at different points of time and not just at a single occasion.
The reasons for these repeated checks are high rate of missed diagnosis on a single clinical examination (especially if the child is irritable) and the now well documented incidence of late-onset dysplasia (hips are normal at birth but turn dysplastic sometime later in infancy).
The guidelines propose hip clinical examination at birth (immediately after birth and at discharge), 6 weeks, 10 weeks, 14 weeks, 6 months, 9 months, 12 months, 15 months and 18 months age.
These timepoints align with vaccination/ well-baby clinic visits as recommended in the National Immunization Schedule.
QUESTION 3: WHICH CLINICAL TESTS SHOULD BE PERFORMED AT EACH SURVEILLANCE POINT?
The minimum clinical tests to be performed at each exam include:
a. For children < 14 weeks age:
i. Ortolani test: This is a clinical test where attempt is made to reduce a dislocated hip. Positive Ortolani test implies that the hip is dislocated at rest but can be reduced on performing the Ortolani manoeuvre.
ii. Barlow test: This is a clinical test where attempt is made to dislocate a reduced hip. Positive Barlow’s test implies that the hip is reduced at rest, but it is unstable and can be dislocated on applying stress by the Barlow’s manoeuvre.
Watch the following video by the International Hip Dysplasia Institute (IHDI), demonstrating the performance of Ortolani and Barlow tests:
b. For children > 14 weeks age:
i. Limited hip abduction: In an infant, hips when flexed to 90 degrees can be abducted sufficiently so that the lateral surface of thigh touches the examination couch. Failure to do so indicates restricted abduction (Figure 4).
ii. Galeazzi sign/ leg length discrepancy (Figure 5).
iii. Limp (in walking age child)

Figure 4: Restricted hip abduction

Figure 5: Galleazzi sign
QUESTION 4: WHAT ARE THE POSITIVE RISK FACTORS FOR DDH?
In addition to clinical examination, the clinician should make note of positive risk factors for DDH. These include:
1-Positive family history
2-History of breech presentation
3-History of restrictive swaddling: Swaddling the baby with hips and knees in forced extension is known as “Restrictive Swaddling”. This is a positive risk factor for DDH.
In contrast, swaddling the baby with adequate space to flex the hips and knees is known as “Hip-Safe Swaddling” and should be encouraged (Figure 6).
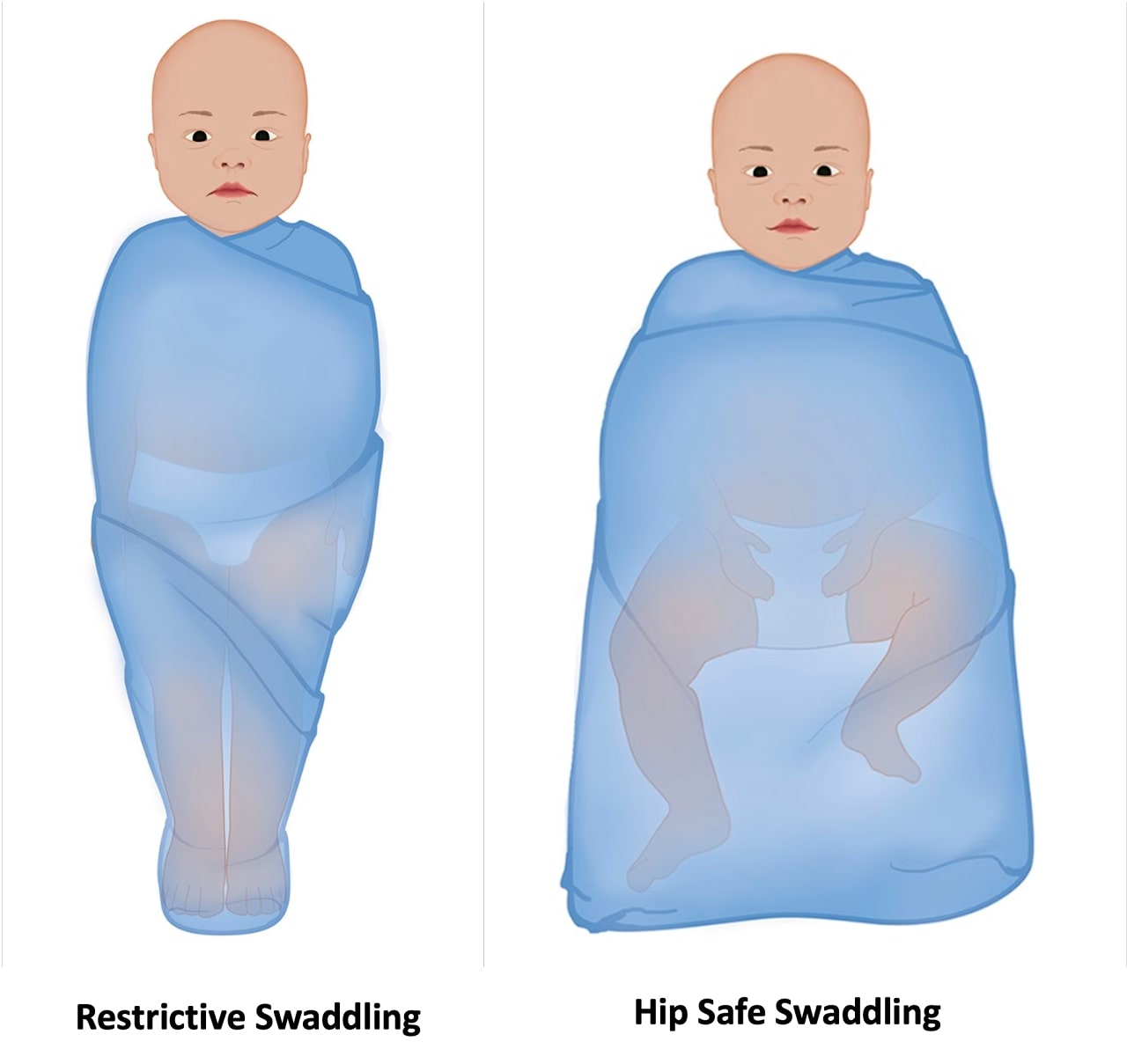
Figure 6: “Restrictive” and “Hip-safe” swaddling
QUESTION 5: WHAT ARE THE INDICATIONS FOR REFERRAL FOR IMAGING?
Referral for imaging is indicated in the following situations:
- Positive Barlow Test: As mentioned earlier, this implies a hip which is reduced at rest, but can be dislocated on application of stress.
- Presence of any of the above-mentioned risk factors for DDH.
- Equivocal findings on clinical examination.
QUESTION 6: WHICH IS THE IMAGING MODALITY OF CHOICE?
The imaging modality of choice depends on the age of the child:
1-For children < 14 weeks age: The imaging modality of choice is an Ultrasonography of the hip joints. The investigation requested is Ultrasonography of both hip joints by Graf’s static method and Harcke’s dynamic method.
2-For children > 14 weeks age: The imaging modality of choice if X-ray Pelvis with both hips Antero-posterior view.
QUESTION 7: AT WHAT AGE SHOULD THE CHILD BE REFERRED FOR IMAGING?
Referral for imaging should be made after the child is 6 weeks old. The reason to wait till 6 weeks age is that performing an Ultrasonography before the age of 6 weeks might over-diagnose a physiologically immature hip as dysplastic thereby leading to inappropriate treatment.
QUESTION 8: WHAT ARE THE INDICATIONS FOR REFERRAL TO ORTHOPAEDIC SURGEON?
Referral to orthopaedic surgeon is indicated in the following situations:
- Positive Ortolani Test: As mentioned earlier, this implies a hip which is dislocated at rest.
- Persistence of Positive Barlow Test beyond the age of 6 weeks.
- DDH diagnosed on imaging studies
CONCLUSION:
The Indian Hip Surveillance guidelines are easily implementable in Indian settings. The next logical step towards the implementation of this program would be raising awareness amongst stakeholders which include all healthcare workers involved in the care of newborns and children.
Successful implementation of this program nation-wide holds the promise of significantly decreasing the disease load of late detected DDH and need for invasive surgery.
_ By Dr Sandeep Vaidya, Paedictric Orthopaedic Surgeon, Pinnacle Orthocentre Hospital. For more information, mail drsvvaidya@gmail.com/ call 7028859555.




0 Comments